
Obesity can cause male infertility, and the reproduction potential can thus be negatively affected, particularly via alteration in the hypothalamic-pituitary-gonadal axis, disruption of testicular steroidogenesis, and also metabolic dysregulation, including insulin, cytokines, and adipokines.
Obesity and male infertility are interconnected in multifaceted ways.
Obesity can indeed significantly impact semen quality and spermatogenesis. It can lead to reduced testicular volume, poor sperm quality, and abnormal sperm morphology.
Sperm count, concentration, and motility can decrease, while the DNA fragmentation index may tend to increase.
Obesity does disrupt the synchronized working of the reproductive-endocrine milieu, particularly the hypothalamic-pituitary-gonadal (HPG) axis.
Altered hormonal profiles (reduced inhibin B and androgen levels accompanied by elevated estrogen levels) do contribute to impaired spermatogenesis.
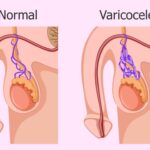
Increased scrotal temperature due to heavy adipose tissue deposits can affect sperm production.

Systemic inflammation and also oxidative stress (OS), initiated by adipose tissue-derived pro-inflammatory mediators, do impact semen quality.
Obesity can indeed modulate sperm genetic and epigenetic conformation, thus disrupting sperm functions.
Paternal obesity has indeed adverse effects on assisted reproductive techniques (ARTs) outcomes as well as offspring health.
Obesity-induced male infertility does entail a complex interplay of physical, endocrine, and genetic factors.
Researchers continue to explore this health issue, seeking timely updates as well as a deeper understanding.
Maintaining a healthy weight is important for male fertility. Even being 20 pounds over the ideal weight does enhance the chances of male infertility. If concerned about fertility, it is rather advisable to consider lifestyle changes and also seek professional advice.
Obesity is rather considered a global health problem, thus affecting more than a third of the population. Complications of obesity do involve cardiovascular diseases, type 2 diabetes mellitus, malignancy (including prostatic cancer), neurodegeneration, and accelerated aging. In males, these further include erectile dysfunction, poor semen quality, and subclinical prostatitis. Although poorly understood, important mediators of obesity that can influence the male reproductive system include hyperinsulinemia, hyperleptinemia, chronic inflammation, and oxidative stress.
Obesity is supposed to disrupt male fertility and reproduction potential, particularly via alteration in the hypothalamic-pituitary-gonadal axis, disruption of testicular steroidogenesis, and also metabolic dysregulation, including insulin, cytokines, and adipokines. Importantly, obesity and its underlying mediators do result in a negative impact on semen parameters, including sperm concentration, motility, viability, and normal morphology. Obesity does inhibit chromatin condensation and DNA fragmentation, which tend to enhance apoptosis and also epigenetic changes that can be transferred to the offspring.
The focus has to be on weight management strategies, lifestyle changes, prescription medication, and complementary and alternative medicine in the management of obesity-induced sub-fertility, etc. if faced with male infertility issues due to obesity.
Obesity does affect female and male fertility and does lead to multiple adverse reproductive outcomes. There are indeed potential adverse effects of female and male obesity, as well as the impact of weight loss on their respective fertility status.
The destructive effects of female obesity on reproduction are attributed to a variety of ovarian and extra-ovarian factors. In women who are overweight or obese, the time taken to conceive is longer, and they indeed have a decreased fertility rate, an increased requirement for gonadotropins, and a higher miscarriage rate when compared to those with a normal weight. Male obesity can lead to sub-fertility, mainly because of the disruption of the hypothalamus-pituitary-gonadal (HPG) axis, increased testicular temperature, impairment of the physical as well as molecular structure of sperm, decreased sperm quality, and erectile dysfunction due to peripheral vascular disease. Most studies do recommend lifestyle interventions as first-line therapy among the general population of women and men with obesity and infertility health issues.







©2024. Andro9. All Rights Reserved.