Peyronie’s disease is worrisome and requires treatment. If in the early stages of Peyronie’s disease, it can be dealt with, but if chronic, then it requires care.
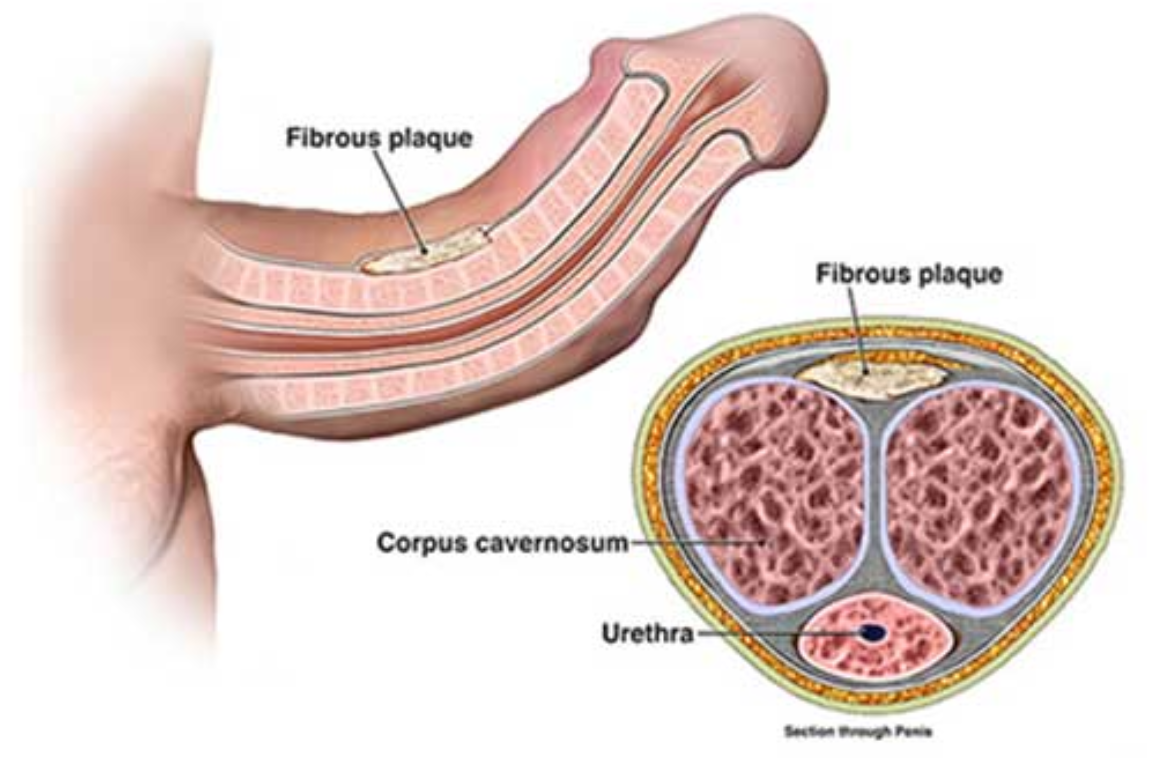
Peyronie’s disease (PD) happens to be an acquired connective tissue disorder of the tunica albuginea of the corpus cavernosum, which is characterized by excessive fibrosis and plaque formation. PD can result in significant physical as well as psychological morbidity, as it may prevent intercourse and also have adverse impacts on partner relationships. The exact etiology as well as pathophysiology remain unclear, and several misconceptions about the disease associations, course, and treatment do exist.
Stages of Peyronie’s disease
The disease has indeed two distinct stages. The acute stage is rather characterized by pain, and disease may progress during this stage. Non-surgical management at this stage does aim to alleviate pain and also stabilize the disease. Results for non-surgical treatment appear often to be conflicting. The chronic stage does occur 6–12 months later, whereby pain tends to disappear and the deformity stabilizes. Surgical treatment is indeed reserved for patients with a significant deformity or an inability to have penetrative intercourse. The choice of the surgical technique does depend on the length of the penis, degree of deformity, erectile function, patients’ expectations, and the surgeon’s preference.
These sorts of misconceptions do represent obstacles to early treatment at the disease-course stage. Studies do show that an earlier age of presentation (40–50 years) and the presence of hypertension, diabetes mellitus, and dyslipidemia do pose a greater risk for early disease progression. Studies also indicate that early detection and treatment can reduce psychological distress. Thus, greater awareness of the natural history and course of PD may in fact promote early detection and prompt treatment of the disease and thus lead to improvement both at the physical and psychological levels of outcomes in these men.
What to know more about Peyronie’s disease?
Peyronie’s disease is indeed a noncancerous condition that does result from the development of fibrous scar tissue on one’s penis, causing curved and painful erections. The condition can lead to bends or pain in a few men, making it quite difficult to get or even maintain an erection. Penile shortening can be another common concern. Peyronie’s disease rarely ends up going away on its own, and in most men with Peyronie’s disease, the condition will remain as it is or worsen. Early treatment soon after developing the condition can keep it from getting worse or even improve symptoms. Even if a person has had the condition for some time, treatment can help improve bothersome symptoms like pain, curvature, and penile shortening.
It is essential to consult a doctor as soon as possible if you notice signs or symptoms of Peyronie’s disease. Early treatment does give a person suffering from it the best chance to improve the condition or even prevent it from getting worse.
How long does Peyronie’s disease last?
Peyronie’s disease, already mentioned, has two stages: acute and chronic. The acute stage does last between six and 12 months. During this period, a scar forms under the skin of one’s penis, causing it to curve or change its shape another way. It can be painful.
What is the difference between acute and chronic Peyronie’s disease?
The acute stage lasts between six and 12 months. During this period, a scar forms under the skin of the penis, causing it to curve or change its shape another way. It can be painful when the penis is erect or soft (flaccid). A chronic condition also needs treatment, and even if the condition is such, treatment can help improve bothersome symptoms like pain, curvature, and penile shortening.
Conclusion
Peyronie’s disease, in fact, rarely goes away on its own. In most men with Peyronie’s disease, the condition remains as it is or worsens. Early treatment soon after developing the condition can thus keep it from getting worse or even improve symptoms.